Oct 24, 2018
The slogan and hashtag of this year’s World Stroke Day is #UpAgainAfterStroke. The SAFE member organisation from Serbia sent us a very inspirational story of a young woman who managed to conquer stroke and kept pursuing her dreams.

Photo: Private archive of Marina Krsmanovic
Marina Krsmanovic from Serbia, a nursery teacher and mother of two, never was a smoker and did sports on regular basis. Despite her healthy lifestyle, in December 2017 she felt that her right arm was paralysed, she lost her sight and she noticed speech difficulties.
She did not wait and she immediately called for help. Within one hour she was admitted to St. Sava (Sveti Sava) Special Hospital for cerebrovascular diseases in Belgrade, Serbia. The medics diagnosed a stroke which was a consequence of a congenital heart disease. She was sent to the Institute of Cardiovascular diseases where she had a heart surgery on 24th January 2018.
She found her motivation and strength for recovery in her children. She adopted a new diet, changed the way of thinking and she now says that she has started enjoying her life, finding happiness in small things and that she always has positive thoughts. It’s safe to say that her fast reaction at the first symptoms, quick transportation to hospital and of course high quality treatment in the above mentioned medical institutions were the key for her successful recovery. Now, she can function independently, she has returned to her workplace…
When we got in touch with her, we heard some great news and it’s not enough to say that we were amazed. Apart from returning to her everyday routine, Marina has returned to her hobby that she practiced before stroke- downhill mountain biking. She even won a medal at a competition that took place on Zlatibor mountain (Western Serbia) at which she was the only female competitor!

Photo: Private archive
She said that her only goal has been to take part in the competition and to prove it to herself that she could tame the mountain once again. Taking part in the competition is worth all the attention and admiration one could get but winning a medal is like reaching the top of the world.

Photo: Private archive
Her message to all of us is stick to positive thinking, enjoy little things and enjoy your life to the fullest. We hope that Marina’s story will motivate people never to give up and to keep fighting. We, on our behalf, have a duty to do everything we can to make life easier for those who had suffered a stroke, to help them get #UpAgainAfterStroke!
If you want to share your experiences with SAFE and if you want set an example for people who are facing a stroke and all its consequences, please contact us via Facebook and Twitter.

Oct 21, 2018
At this year’s World Stroke Congress In Montreal, Canada, SAFE was present through a variety of activities, from chairing stroke support sessions, being one of the key speakers and presenters, having a very well noticed and visited information stand, to actively participating in the World Stroke Day workshop and shaping the World Stroke Campaign in the years to come.
SAFE President Jon Barrick presented the SSOFT project, an online ‘how to’ toolkit for a range of advocating skills training, from setting up a stroke support organisation to leading PR and advocacy campaigns. This tool aims to build capacity of the European SSOs but can be used much broader to increase one world voice for stroke. His presentation sparked interest even among SSOs from other continents leading to an interesting exchange of ideas and suggestions for its further development. The SSOFT project will be completed by end of November 2018. Project team are looking at the future development such as translation into other languages, additional modules, global scope, said Barrick, but it is depending on funding. The presentation was broadcasted live on Facebook and the video can be found here.
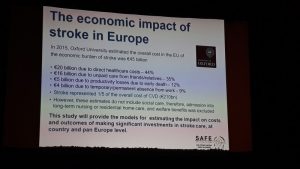
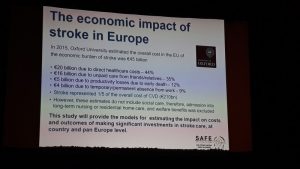
In addition to the SSOFT project, SAFE had a chance to present the economic Burden of Stroke Report, scheduled to be published towards the end of 2019, as well as the SAFE & Industry Partner collaboration project on Life With Spasticity.
 However, the Stroke Action Plan for Europe 2018-2030, a joint SAFE and ESO project got the majority of attention due to the fact that it just has been launched in May this year and is aimed to set the road map for stroke prevention, treatment and life after stroke in Europe in the next 12 years.
However, the Stroke Action Plan for Europe 2018-2030, a joint SAFE and ESO project got the majority of attention due to the fact that it just has been launched in May this year and is aimed to set the road map for stroke prevention, treatment and life after stroke in Europe in the next 12 years.
Successful examples and case studies from around the world, such as the one of the Swedish Stroke Registry and their latest project about caregivers and how they are coping with the consequences of strokes in their loved ones. The need for comprehensive and systematic follow up reviews for stroke survivors, after 3, 6 and 12 months was particularly stressed out.

Prof. Bo Norrving
We heard from Prof. Bo Norrving, University of Lund, Sweden, that one of 6 strokes was eradicated in Sweden over the last 6 years, meaning 14,000 in absolute number of strokes, and saving one billion euros. The reason for this success lays in treatment of TIA, atrial fibrillation and use of preventive medications. Stroke is probably the single most preventable disease of all. It may be that I am wrong, but I would like to be proven to be wrong, said Prof. Norrving.
During a separate open session on stroke as part of the non-communicable disease, Stephanie Mohl on behalf of American Heart and Stroke Association opened the conversation saying: Here we are in 2018 and we still need to talk about why patients need to in center of the healthcare, pointing towards all of the necessary efforts to convince the policy decision makers to listen to the patient voice in almost all parts of the world.
The way non-communicable diseases were addressed so far by the policy makers, the NCD acronym might as well stand for No Can Do, said Jon Barrick. This needs to be changed, but we need to be aware that people don’t put energy into hopeless campaigns, so stroke support organisations should be more active in showing perspectives and opportunities for stroke survivors and their carers.
SAFE was active on social media during the whole three days of the World Stroke Congress. For more information, please visit our social media accounts on Facebook and Twitter.

An open session on stroke and non-communicable diseases

Oct 14, 2018
The story first appeared on ScienceDaily.com
New findings suggest that diet is a major contributor for the increased risk of hypertension in black compared to white Americans. The results, published in the Journal of the American Medical Association, are part of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, which looks at the incidence of stroke in approximately 30,000 individuals. The study is funded by the National Institute of Neurological Disorders and Stroke (NINDS), a part of the National Institutes of Health.
“This study addresses a lead cause of racial disparity in mortality and identifies potential lifestyle changes that could reduce racial disparities in both stroke and heart disease,” said Claudia Moy, Ph.D., NINDS program director and one of the study authors.
In the study, led by George Howard, Dr.P.H., a biostatistics professor at the University of Alabama at Birmingham, researchers studied individuals over the age of 45 over a period of 10 years and looked to identify risk factors associated with the higher likelihood of developing high blood pressure in the study participants.
“The majority of disparities we see in the health of black versus white Americans are cardiovascular in nature,” said Dr. Howard, “and of these, all are tied to an increase in high blood pressure.”
For both men and women, a diet composed of high amounts of fried and processed foods and sweetened beverages was the greatest factor associated with why blacks are at a greater risk of developing high blood pressure compared to whites. For both men and women, other important factors included salt intake and education level. For women, additional factors contributing to the racial difference in high blood pressure included obesity and waist size.
“One of the main factors affecting the difference between the black and white population is cardiovascular disease, and the increased risk of high blood pressure among black Americans could help explain why their life expectancy is four years shorter than that of whites,” said Dr. Howard. “Understanding how we can prevent this increased risk of hypertension in blacks is critical for reducing health disparities among the black population.”
The researchers hope that these findings could be applied to reduce the prevalence of hypertension and thus the risk of stroke and heart attack in the black American population. This study suggests that lifestyle changes, particularly changes in diet, could help reduce the disparities seen in black versus white Americans.
“The best way to treat high blood pressure is to prevent it from occurring in the first place,” said Dr. Howard.
The REGARDS study includes more than 30,000 black and white Americans, approximately half of whom live in the Stroke Belt, an area in the southeastern United States where the rate of stroke mortality is higher than the rest of the country. Of these, 6,897 participants, 1,807 black and 5,090 white, were analyzed for this study.
In 2016, the NINDS launched a stroke prevention campaign called Mind Your Risks, which is designed to educate people aged 45-65 about the link between uncontrolled high blood pressure and the risk of having a stroke or developing dementia later in life.
Story Source: NIH/National Institute of Neurological Disorders and Stroke. “Diet rich in fried and processed foods linked to increased hypertension in black Americans: Study suggests a change in diet could mitigate increased risk for stroke.” ScienceDaily. ScienceDaily, 3 October 2018. <www.sciencedaily.com/releases/2018/10/181003193936.htm>.

Oct 5, 2018
As World Stroke Day 2018 approaches, we would like to invite you to register your event on the World Stroke Campaign website, by clicking on this button below.
Registration link WSD 2018
SAFE is proud of our member organisations who did tremendous work around World Stroke Day 2017, wholeheartedly supporting the “What’s your reason?” campaign. through use of texts, visuals and other material produced by WSO for this purpose.
We also used the opportunity to convey our own messages based on the Burden of Stroke in Europe Report findings, related to the lack of prevention and stroke awareness campaigns in Europe, as well as the underestimated danger coming from the three biggest stroke risk factors- blood pressure, AF and high cholesterol.
Whether it was a series of lectures like in Cyprus, Portugal, or a book promotion in Luxembourg or sports events that our colleagues from Ireland, Poland and many other countries organised- we showed that raising awareness of stroke was an important topic. Many of our organisations start the preparation for the World Stroke Day long before 29th October. For example, our colleagues from Slovenia started with activities dedicated to WSD as early as September by attending the Festival for the third age and with September’s national gathering, having a stand and giving a free lecture on how to beat stroke, delivered by the vice-president of the Slovenian Stroke Support Organisation, dr. Tatjana Erjavec.
What is your plan for this year? Register your event, put yourself on a map of stroke activists from around the world.

Oct 3, 2018
From the beginning of the Stroke Support Organisation Faculty Tool (SSOFT) project the needs of the members of the Stroke Alliance for Europe (SAFE) has been central to the whole process.
The needs of the people who would use SSOFT, was a focus at the last SAFE Working Conference in Zagreb (December 2018) where half a day was dedicated to gaining insight and feedback from the numerous member who attended. One of the many SAFE members who were enthused by this project and volunteered to be part of the User Acceptance Testing Group was Nenad Nikolić from Moždani Udar, the Serbian Stroke Association.
Nenad has worked as a Medical Technician in a Neurology ward in the General Hospital in Ćuprija Serbia, for the past 15 years where he has worked with many stroke patients over the years. Nenad became an active member of the Serbian Stroke Association due to his own personal experience, when his mother suffered a stroke ten years ago.
We caught up with Nenad at the SAFE Regional Conference in Prague to ask him about his SSOFT experience so far.
When SSOFT was presented at the SAFE Working Conference last year what sparked your interest?
SSOFT attracted my attention as I wanted to see how it fitted with my experience as a medical technician working with stroke patients. I saw the potential for this tool as a valuable resource and therefore I volunteered to become a tester of SSOFT. I also had a strong personal motivation to participate as I wanted to learn more about advocacy to help further develop our SSO’s activities.
How have you found the User Acceptance Testing process?
All in all, testing this tool is a very interesting experience and much can be learned.So far, I have tested four out of six modules and after each testing session I have sent my observations and recommendations to the project team. I have had a lot of ideas and recommendations which I shared with the team and I am pleased to say a lot of them have been accepted. The opinion of the people who test the program is important. Therefore, SSOFT is exactly what should be: a tool “for our members by our members”.
Can you briefly describe SSOFT to those who haven’t used it yet?
SSOFT is an e-learning toolkit for organisations that deal with stroke. SSOFT aims to provide the necessary information for effective local and national campaigns to improve prevention, recognition, treatment and care of stroke. SSOFT will have six modules which are in smaller sub-sections which displays the information on slides, like a PowerPoint presentation. The modules also have a lot of video materials where members of stroke organisations or stroke survivors share their experiences, which is certainly of great help. The video clips are in English and are easy to understand. There are also activities and quizzes which keeps things interesting. It is very interactive.
What is your overall impression of SSOFT?
My general impressions are very good, and I find that the entire interface simple and easy to use. The text is easy to read and see, there is also sound that follows the text (a voiceover in English language). All audio-visual content is understandable and can be easily used by people who have suffered stroke, which is very important.The language used is simple, without too many medical terms, so non-medical worker will understand it. As far as content is concerned, it’s very useful and it has plenty of valuable information (from what it takes to start the local Stroke Support Organisation, to recommendations for successful campaigns). From what I have seen so far, I can say that the content “hits the target”.
Would you recommend other people use SSOFT?
Of course! If you are stroke survivor or carer or member of an organisation which deals with stroke, SSOFT is a valuable resource with plenty of useful information about how to advocate for either better stroke prevention or treatment or long-term care.

Oct 3, 2018
Cells and platelets stick inside arteries, increase risk after initial attack
The original article was first published on ScienceDaily.com
Doctors have long known that in the months after a heart attack or stroke, patients are more likely to have another attack or stroke. Now, a paper in the Journal of the American College of Cardiologyexplains what happens inside blood vessels to increase risk — and suggests a new way to treat it.
Heart attacks in mice caused inflammatory cells and platelets to more easily stick to the inner lining of arteries throughout the body — and particularly where there was already plaque, according to the paper. As a result, these sticky cells and platelets caused plaque to become unstable and contribute to blood clots that led to another heart attack or stroke.
But the study found treating mice that had experienced a heart attack or stroke with the powerful antioxidant apocynin cut plaque buildup in half and lowered inflammation to pre-attack levels.
“Knowing that newer forms of antioxidants such as apocynin can lower the risk of a second heart attack or stroke gives us a new treatment to explore and could one day help reduce heart attacks and strokes,” said the paper’s corresponding author, Jonathan R. Lindner, M.D., a professor of cardiovascular medicine at the OHSU School of Medicine.
Lindner penned the research paper with colleagues from OHSU, Scripps Research Institute and Bloodworks NW.
The researchers discovered the sticky cells and platelets by using unique forms of ultrasound imaging they developed to view molecules on the lining of blood vessels.
This research could help explain why the recent Canakinumab Anti-inflammatory Thrombosis Outcomes Study, also known as the CANTOS clinical trial, found an anti-inflammatory drug already approved to treat juvenile arthritis also reduced the risk of a second heart attack in trial participants by 15 percent.
Lindner and his colleagues are further studying how the relative stickiness of remote arteries affects the risks for additional heart attacks and strokes and are also evaluating new therapies beyond antioxidants.
The study was supported by the National Institutes of Health (R01-HL078610, R01-HL130046, R01-HL091153, R01-HL11763, HL42846, HL78784), NASA (grant 14-14NSBRI1-0025) and the Swiss National Science Foundation.
Story Source: Oregon Health & Science University. “Antioxidant reduces risk for second heart attack, stroke: Cells and platelets stick inside arteries, increase risk after initial attack.” ScienceDaily. ScienceDaily, 4 September 2018. <www.sciencedaily.com/releases/2018/09/180904164639.htm>.

Sep 28, 2018
Published by ESO | 25.9.2018
This statement was jointly prepared by the World and European Stroke Organizations (WSO and ESO), the World Federation and the European Academy of Neurology (WFN and EAN) all of which are specialty societies for neurology and brain health.
Statement
NCDs continue to increase worldwide. Cardiovascular diseases, stroke and dementia are a major concern. Stroke is now ranked the 2nd greatest cause of both disability and death worldwide.
Stroke threatens everyone. Stroke causes paralysis of limbs, impairs vision, gait, language and cognition. It contributes to dementia. Of particular concern is the increasing stroke burden in young adults and its effect on keeping employment, as more than 40% of working age adults with stroke fail to return to work.
The burden of stroke disproportionately affects people living in countries with limited resources, also in Europe. Most stroke survivors carry lifelong physical, cognitive, mental, and socio-economic burdens. A significant proportion of European and Global NCD burden can be attributed to stroke and stroke-related dementia. This issue of NCDs, including stroke and dementia, is highlighted at this month’s UN High Level Meeting in New York.
The importance of stroke is acknowledged by the WHO in ICD 11 where stroke is now included as a disease of the nervous system. This most important change will have dramatic impact on the promotion of brain health and the distribution of resources.
For stroke prevention, it is important to know that 90 % of strokes are linked to 10 modifiable risk factors including hypertension, smoking, obesity, physical inactivity, and unhealthy diet. The same factors apply to ischemic heart disease, the other main cause of global disability and death. The occurrence of an acute stroke has to be considered a major emergency which needs a seamless chain of interventions until recovery. Quality care needs to be provided timely by competent personnel and teams across the whole pathway in an organized and audited manner. This kind of access to adequate stroke expertise should be independent of region, time of day and socio-economic status. These stroke facts were highlighted during last year’s WFN World Brain Day.
Dementia on the other hand is growing globally with ageing populations, and stroke contributes with other NCDs such as hypertension, heart disease, chronic kidney disease and diabetes mellitus to the development of dementia. Rates of dementia may be reduced by modifying these risk factors and both stroke and dementia may be prevented through coordinated action.
Developments in vascular neurology has made stroke and dementia preventable, treatable and increasingly reversible, thus reducing the burden on patients, families and societies. To ensure these developments are more evenly distributed, we will require national, regional and global efforts to increase awareness, make available quality acute stroke treatment, primary and secondary prevention and rehabilitation.
ESO and the patient organization SAFE (Stroke Action for Europe – https://www.safestroke.eu) have just finalized the Action Plan for Stroke in Europe 2018-2030, which is aligned with the UN’s Sustainable Development Goals. The plan has four overarching goals:
1) to reduce the absolute number of strokes in Europe by 10%
2) to treat 90 % or more of all patients with stroke in Europe in a dedicated stroke unit as the first level of care
3) to have national plans for stroke encompassing the entire chain of care, and 4) to fully implement national strategies for multisector public health interventions In this context WSO, ESO, EAN and WFN call upon the WHO European Regional Committee to support its member states to increase their efforts based on these three domains:
Awareness: WHO-Europe should help to strengthen programs that increase awareness of stroke, as risk factors, therapy and rehabilitation.
Access: We will support WHO-Europe with its efforts to remove financial barriers for patients for prevention, detection and treatment of NCDs, including European wide health coverage.
Action: The neurology specialist societies will support WHO-Europe in the development of regional and national strategies, to develop the health-relatedSustainable Development Goals, with the goal to reduce premature deaths caused by NCD by one-third by 2030.

Sep 28, 2018
First appeared on ScienceDaily.com
A novel therapy technique invented by researchers at The University of Texas at Dallas has been shown in a pilot study to double the rate of upper limb recovery in stroke patients, a leap forward in treating the nearly 800,000 Americans who suffer strokes each year.
The results of the study, funded by UT Dallas spinoff company MicroTransponder of Austin, Texas, were published Sept. 27 in the journal Stroke.
The findings indicate that targeted plasticity therapy — which involves stimulation of the vagus nerve — paired with traditional motor-skill rehabilitation is not only safe, but also twice as effective as rehab alone.
Dr. Jane Wigginton, the chief medical officer at UT Dallas’ Texas Biomedical Device Center (TxBDC) and an associate professor of emergency medicine at UT Southwestern Medical Center, led the Dallas site of the clinical trial, which involved 17 people across the country who had suffered a stroke.
“Stroke is too common and too debilitating for us to tolerate the status quo,” Wigginton said. “Patients need a real solution so they can get back to fully living their lives.”
Dr. Michael Kilgard, associate director and chief science officer of the TxBDC, invented targeted plasticity therapy (TPT). Kilgard, who is also the Margaret Fonde Jonsson Professor in the School of Behavioral and Brain Sciences (BBS), said the study results further validate the theories that he and his colleagues based their TPT work on beginning in 2009.
“We set out to design an approach that could transform long-term care and restore quality of life to patients for whom that has thus far been impossible,” said Kilgard, who was not involved in the clinical trial. “These results show our method has immense potential. We’re excited about what this could mean for millions of stroke patients worldwide.”
Researchers affiliated with the TxBDC and BBS developed the therapy technique, which pairs physical movements with precisely timed vagus nerve stimulation (VNS) — electrical stimulus of the nerve via a device implanted on the nerve in the neck.
The vagus nerve controls the parasympathetic nervous system, overseeing many unconscious functions such as circulation and digestion. Stimulating the nerve initiates neural plasticity — reorganization of the brain’s circuitry. The idea behind TPT is that synchronizing VNS with movement accelerates plasticity in a damaged brain, and with it, recovery.
A stroke occurs when blood flow to the brain is interrupted because of a blockage or a ruptured blood vessel. Limb mobility can be affected when nerve cells are damaged. Such forms of brain trauma are often treated with rehabilitation that includes repeated movement of the affected limb in an effort to regain motor skills. The approach is thought to work by helping the brain reorganize.
Several studies of Kilgard’s technique in animal models have previously demonstrated that it is effective in recovering limb function after stroke. A small clinical trial in Europe also provided encouraging data for its potential use in humans.
In 2009, UT Dallas licensed its VNS technique as a stroke and tinnitus treatment to MicroTransponder, which sponsored the new double-blind, placebo-controlled study. Neither the researchers nor the study subjects knew who was getting VNS stimulation and who was not.
Each study subject was a stroke patient whose stroke occurred between four months and five years prior to selection. After they had a VNS device implanted, the subjects received six weeks of in-clinic rehab followed by a home exercise program. About half were treated with active VNS while the rest received control VNS. All were assessed one, 30 and 90 days after therapy with a widely used, stroke-specific measure of performance impairment.
In addition to showing that the technique is safe, the researchers found that subjects receiving active VNS scored more than twice as high as control subjects at the 30- and 90-day intervals, opening the way for larger, more extensive clinical trials, Kilgard said. One such trial is in the recruitment phase and includes a study site in Dallas.
Story Source: University of Texas at Dallas. “Enhanced rehab for stroke doubles movement recovery.” ScienceDaily. ScienceDaily, 27 September 2018. <www.sciencedaily.com/releases/2018/09/180927083333.htm>.

Sep 20, 2018
The original article first published on ScienceDaily.com
One of the largest and longest-running efforts to evaluate the potential benefits of the Mediterranean-style diet in lowering risk of stroke found that the diet may be especially protective in women over 40 regardless of menopausal status or hormone replacement therapy, according to new research in the American Heart Association’s journal Stroke.
Researchers from the Universities of East Anglia, Aberdeen and Cambridge collaborated in this study using key components of a traditional Mediterranean-style diet including high intakes of fish, fruits and nuts, vegetables, cereal foods and potatoes and lower meat and dairy consumption.
Study participants (23,232 white adults, 40 to 77) were from the EPIC-Norfolk study, the United Kingdom Norfolk arm of the multicenter European Prospective Investigation into Cancer study. Over a 17-year period, researchers examined participants’ diets and compared stroke risk among four groups ranked highest to lowest by how closely they adhered to a Mediterranean style diet.
In participants, who most closely followed a Mediterranean-style diet, the reduced onset of stroke was:
- 17 percent in all adults;
- 22 percent in women; and
- 6 percent in men (which researchers said could have been due to chance).
“It is unclear why we found differences between women and men, but it could be that components of the diet may influence men differently than women,” said Ailsa A. Welch, Ph.D., study lead author and professor of nutritional epidemiology at the University of East Anglia, United Kingdom. “We are also aware that different sub-types of stroke may differ between genders. Our study was too small to test for this, but both possibilities deserve further study in the future.”
There was also a 13 percent overall reduced risk of stroke in participants already at high risk of cardiovascular disease across all four groups of the Mediterranean-diet scores. However, this was driven mainly by the associations in women who showed a 20 percent reduced stroke risk. This benefit appeared to be extended to people in low risk group although the possibility of chance finding cannot be ruled out completely.
“Our findings provide clinicians and the public with information regarding the potential benefit of eating a Mediterranean-style diet for stroke prevention, regardless of cardiovascular risk,” said Professor Phyo Myint, M.D., study co-author and former British Association of Stroke Physicians Executive Committee member, University of Aberdeen, Scotland.
“A healthy, balanced diet is important for everyone both young and old,” said Professor Ailsa Welch.
Researchers used seven-day diet diaries, which they said had not been done before in such a large population. Seven-day diaries are more precise than food-frequency questionnaires and participants write down everything they eat and drink over the period of a week.
“The American Heart Association recommends a heart-healthy and brain-healthy dietary pattern that includes a variety of fruits and vegetables, whole grains, low-fat dairy products, fish, poultry, beans, non-tropical vegetable oils and nuts and limits saturated fat, trans fat, sodium, red meat, sweets and sugar-sweetened beverages; this dietary pattern reduces risk factors and risk for heart disease and stroke, “said Eduardo Sanchez, M.D., MPH, the American Heart Association’s chief medical officer for prevention and chief of the Association’s Centers for Health Metrics and Evaluation, who was not a part of this study. “This study provides more evidence that supports AHA’s recommendation,” said Sanchez.
Story Source: American Heart Association. “Mediterranean-style diet may lower women’s stroke risk.” ScienceDaily. ScienceDaily, 20 September 2018. <www.sciencedaily.com/releases/2018/09/180920075854.htm>.
Sep 18, 2018
Conducted by King’s College London on behalf of SAFE in May 2017, the Burden of Stroke Report has now been translated into Greek language. Manuscript translation editing was done by Hariklia Proios, PhD CCC-SLP, Ast. Professor of neurocognitive sciences and rehabilitation, Anna Tsiakiri, PhD Psychologist, Aikaterini Kiriakidou, MD Special Neurologist, Konstantinos Charalampopoulos, MD PhD Special Neurologist and Kalliopi Tsakpounidou, MSc PhD Candidate.
The book will be distributed to the public by the H.N.S.-Hellenic Neurological Society (H.N.S.), the Hellenic Neuropsychological Society (H.NP.S.), the Hellenic Society of Vascular and Endovascular surgery (H.S.V.S.) and the Hellenic (Greek) Stroke Society (Hellenic Society of Cerebrovascular Diseases).
It was presented for the first time in August 31st, 2018, in the board meeting of SAFE in Grand Hotel Palace in Thessaloniki, Greece and will be published by EKDOSEIS GUTENBERG, Printing & Publishing Company – Athens. The aim of the publication is to inform Greek society about the burden of stroke and decrease the rate of this health emergency.






 However, the Stroke Action Plan for Europe 2018-2030, a joint SAFE and ESO project got the majority of attention due to the fact that it just has been launched in May this year and is aimed to set the road map for stroke prevention, treatment and life after stroke in Europe in the next 12 years.
However, the Stroke Action Plan for Europe 2018-2030, a joint SAFE and ESO project got the majority of attention due to the fact that it just has been launched in May this year and is aimed to set the road map for stroke prevention, treatment and life after stroke in Europe in the next 12 years.