
May 3, 2019
This year, SAFE Regional Conferences will be held in Paris on Thursday May 9th, Krakow on Wednesday June 12th and Stockholm on Wednesday June 26th.
SAFE member organisations from 30 European countries will gather within their clusters to discuss the following items:
- A review of SAFE’s work, including the updating of its strategy and a discussion of its relationship with, and activities addressing the importance of co-morbidities
- Discussion of the implementation of the Stroke Action Plan for Europe, focusing particularly on work that can be done in each country and stakeholder engagement and partnership in advocacy
- An update on the Romanian Presidency event
- Translations of materials and promotion of the prevention website
- Utilisation of the SSOFT website to enable growth of SSOs and more effective advocacy
- Preliminary findings and messages arising from the Economic Impact of Stroke research
- SAFE Research Projects
- SAFE and World Stroke Day 2019
- Round-up of activity from attending members
SAFE is thankful to Boehringer Ingelheim for the continued sponsorship of our Regional Conferences.

May 3, 2019
“Our country is small in population, around 7 million in total, but we are among the countries with the highest stroke incidence. Approximately 25.000 strokes occur every year in Serbia. With numbers as high as this, a person would think that we are getting closer to a solution of how to take care of those who survive stroke, but the reality is- we are still very, very far from it. As the Stroke Action Plan for Europe 2018 – 2030 stated, the issues that stroke survivors are facing long term have historically been ignored, and this is what we are hoping to see changed, with the implementation of this Plan, over the next 10-12 years” says Dr Ivan Milojević, Vice President of the Serbian stroke organisation “Moždani udar” and SAFE Board member.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
IM: One of the basic things we consider as the biggest problem in Serbia is the nonexistence of an organized service which would deal with patients after stroke. In our country there is a rehabilitation that involves active participation of medical institutions up to 3 months after stroke and later after that patients are left on their own, or to their families. Even if there is an early rehabilitation provided shortly after stroke in the stroke units, and rehabilitation provided later after that in rehabilitation centres and specialized physical rehabilitation facilities, that is not enough, and stroke survivors long term needs for rehabilitation after stroke are not satisfied. Apart from regular check-ups by a neurologist, there are no other forms of organized monitoring of stroke survivors.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
IM: One of the main ideas that led to forming our association was, among others, about finding a way to organise stroke survivors’ gatherings, so they could share their experiences as peer to per support, and to include them in social activities. We tried to form Stroke clubs, and we are still working on finding the most suitable way to organise this activity. Unfortunately, this is not easy, because our organization is small and doesn’t have financial susatainability that would enable us to have our own space or to rent one for this type of gatherings. Our association has an active two-way communication with stroke survivors via our social network pages. They share with us their stories and we share them through our website and social media channels. We hope these stories might inspire and encourage other stroke survivors to overcome their problems. In that way, and by organizing public campaigns and actions, we are helping the voice of patient to be heard.
SAFE: Please tell us more about your organisation.
IM: Association “Moždani udar” was founded on 30th July 2012 as an NGO. As representatives of stroke patients, we are dedicated to raising awareness of all aspects of stroke. We are involved in many activities and campaigns that cover primary prevention, stroke symptoms early recognition, stroke treatment, rehabilitation, and life after stroke. We were and are part of European and World stroke campaigns, as well as some of the most prominent European projects (Angels Initiative, Stroke Support Organisation Faculty Tool – SSOFT etc). We also share an up-to-date progress information of EU funded stroke research projects by disseminating materials on our language.
Apr 30, 2019
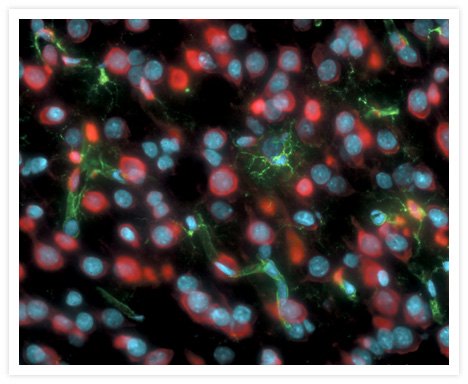
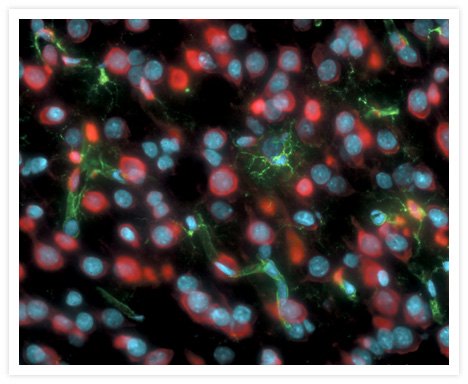
The University of Luebeck is coordinating a new Marie Curie Innovative Training Network called “ENTRAIN”. The project is being funded by the EU commission with 3.6 Mill Euro. Thirteen partner organizations from academia and industry in 9 European countries will be investigating inflammatory processes in the brain, especially those associated with stroke, Alzheimer disease and multiple sclerosis. ENTRAIN follows the project “nEUROinflammation”, which had been funded by the EU since 2013 and was successfully completed in 2017.
The results of nEUROinflammation lead the group to investigate the interactions of specific cell types in the brain, called endothelial cells and microglia, in the current project. The outcome has the potential to improve the therapy of stroke, Alzheimer disease and multiple sclerosis.
The international project will run for 4 years. It aims to support the education of PhD students and to strengthen scientific cooperation in Europe. All in all, 14 postgraduates will work in the research institutions of the partners and participate in workshops and trainings. They will also spend up to 6 months in other partners’ laboratories.
The consortium members of „ENTRAIN“ include the University of Luebeck (Germany), the University Bern (Switzerland), the Westfälische Wilhelms-University Münster, the University Medical Center Freiburg, the Eidgenössische Technische Hochschule Zürich (Switzerland), Stichting VUMC (Netherlands), the Hungarian Academy of Science (Hungary), die Universita Degli Studi di Brescia (Italy), die Universite de Caen Basse-Normandie (France), the Istituto di Ricerche Farmaco-logiche Mario Negri (Italy), the University of Helsinki (Finland), the Agenca Estatal Consejo Superior de Investigaciones Cientificas CSIC (Spain) as well as the company Mimetas BV(Netherlands). The research consortium will be supported by the companies Boehringer Ingelheim GmbH & Co. KG, Brendinn Therapeutics, Dualsystems Biotech AG and Polygene AG as well as the patient organizations Incontinetia Pigmenti France und Stroke Alliance for Europe. Leading experts from these institutions will supervise the PhD students.
Prof. Dr. Markus Schwaninger, Institute for Pharmacology and Toxicology, University of Luebeck, will serve as project coordinator. Susanne Zimmermeier will cover administrative aspects and Dr. Walter Häuser will organizes trainings and workshops for the PhD students; both are also located at the Institute for Pharmacology and Toxicology, University of Luebeck.
Overall there are 14 individual projects involving 14 postgraduates. Two of these projects are based in the Institute for Pharmacology and Toxicology at the University of Luebeck: „Brain macrophages in the remodelling of microvessels“under the supervision of Markus Schwaninger and „Brain endothelial signalling and its regulation by myeloid cells“ under the supervision of Jan Wenzel.
The project starts on May 1st, 2019. At that time the new homepage www.itn-entrain.eu will be launched. There you can find details of the project and candidates will have the possibility to apply online.
The Marie Skłodowska-Curie actions gives universities, research institutions and industrial companies the opportunity to apply for a funding to set up a European network for the structured education of young researchers to support cross-border and cross-sectoral mobility of researchers and to improve their career advancement and knowledge exchange.
The featured image description and credits: Capillary endothelial cells and microglia in a rat brain cryosection, website ThermoFisher Scientific.
Apr 29, 2019
Too many people affected by stroke aren’t getting the support they need. As a charity, the Stroke Association UK knew they needed to reach more people.
On Friday 26 April they have launched their first ever TV-led marketing campaign, Rebuilding Lives.
Rebuilding Lives is aimed to change the way people think about stroke using the real life stories of stroke survivors. Told in their own words. Unscripted. Unfiltered. It is directed by award-winning director Lotje Sodderland, who is herself a stroke survivor. The stories told show that stroke can strike anyone at any time, changing lives in an instant, but that life after stroke is possible. With the right specialist support and a ton of courage and determination, people can recover and adjust to a new normal. The Stroke Association is there to support people to rebuild their lives after stroke.
For more information, please visit https://www.stroke.org.uk/rebuilding-lives

Apr 25, 2019
“Currently, in Portugal, when a stroke occurs, the first phase of treatment, the acute phase, happens in similar conditions to the ones of the best practices in Europe. The first rehabilitation, still within a hospital circle, is already implemented with great differences across our country, and, on average, isn’t as satisfactory. After… when the real life after stroke begins, the survivors and care givers, generally, feel alone, helpless! It’s mostly in that moment, when the biggest problems start (including the psychological, socioeconomic, life reorganization, etc. ones), that, in most cases, there are flaws. Not only in the continuity of the strictly therapeutic recovery, but also in the social and psychological support, among others…” says António Conceição, President of the Portugal AVC, a stroke support organisation that is part of SAFE.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
AC: In Portugal, above all, it’s necessary to remind people, specially people with influence (not only political but other), that survivors have a life after stroke! That they can be active and useful citizens just like everyone else. And an essential contribution for that is making rehabilitation possible and accessible to everyone, as well as making it starts fast, timely and multidisciplinary (since it needs to involve multiple medical and therapeutic areas, that don’t restrict themselves to the physical or motor situation).
 SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
AC: Our procedure, especially in our possibilities of public intervention, has been directed towards two themes: life after stroke and the defense of a better rehabilitation. Recently, we celebrated in Portugal the National Day of Stroke Survivor (31st March). All of our communication, including the one on social communication, followed this line of work: the defense of a fast, timely and multidisciplinary rehabilitation. We pointed out some very concerning flaws. The Portuguese Stroke Society (a medical and scientific organization) also followed an identical theme in its communication. Furthermore, the president of this society, a very prestigious person, said a sentence, a few years ago, that we also repeat many times: “Rehabilitation isn’t a charity, but a right! If needed, during the entire life!” We have conscience that our action has contributed to give prominence to this subject too.
Deeply connected to this theme is the defense of life after stroke, with the maximum quality possible, and the Action Plan for Stroke, by giving the proper importance to life after stroke, has helped us in this struggle. In Portugal, for initiative of the Portuguese Stroke Society, we are working on adapting this plan to our national situation. Unfortunately, we are aware that our action is only starting…
SAFE: Please tell us more about your organisation.
AC: Portugal AVC is a national association, made of stroke survivors, but also of caregivers and health professionals, founded in September 2016. Working like this, we have been functioning very well.
We have, as statuary goals, to contribute to the prevention of stroke and to respond to the needs felt by stroke survivors and their caregivers. And we defined three areas of action as priority:
– Making information available, about all “stages” of stroke, from the prevention to the life after stroke.
– To be the voice of survivors and caregivers, in the government entities and social communication.
– Mutual help. By giving answer to the multiple requests we receive, including by telephone, email, Facebook, … But also, we have promoted and supported the appearance of Support Groups (GAMs). We have already 14, in different places in the country.
Among other activities, we highlight the “Portugal AVC Meetings”. They are moments of interaction with the survivors, caregivers and health professionals, that have had a strong adherence and fantastic environment. We already organized seven, always in different locations, from the north to the south of the country.
However, we are aware that, considering the needs, we are only beginning…

Apr 23, 2019
Atrial fibrillation (AF) is an irregular heart rhythm with rapid and irregular beating. It is estimated to increase the risk of stroke 3 to 5-fold and to be associated with around a quarter of all ischaemic strokes. Additionally, AF is associated with more severe strokes leading to higher mortality and disability. We have discussed this topic with Prof. Dr Anita Arsovska, University Clinic of Neurology, Medical Faculty, University “Ss Cyril and Methodius”, Skopje, North Macedonia, FESO, SAFE Board Member.

Apr 19, 2019
Portugal AVC, stroke support organisation and a member of SAFE, recently published a collection of 21 life stories of stroke survivors. We present you the text that Portugal AVC President, António Conceição, shared with us on this occasion.
…
Author: António Conceição
 We started with posting on Facebook 2 or 3 testimonies, that arrived to us, of people describing their post-stroke life. We quickly realized that these were the most read posts and that they had incredible reactions: We were contributing, with concrete examples, all very different among them, to the motivation of other stroke survivors!
We started with posting on Facebook 2 or 3 testimonies, that arrived to us, of people describing their post-stroke life. We quickly realized that these were the most read posts and that they had incredible reactions: We were contributing, with concrete examples, all very different among them, to the motivation of other stroke survivors!
That way, throughout the next year, we challenged some survivors and caregivers to give their testimony. With completely different life stories, some of them truly difficult, but with something in common: to show how it is possible, even with adaptations, to rebuild a life and reach happiness again!
We have gathered 21 life stories, available on our website, truly extraordinary, with different ages, circumstances and time passed after the stroke. All of this with a worry in the background: to take strength where it seems to lack!
We thought about putting into paper these amazing life stories, to make them more accessible, and in a lasting way. We found a writer of children’s books, a psychiatrist that doesn’t practice, an extraordinary and very sensible person, and we challenged her to compile all of these testimonies, with total respect for the story and style of each person.
Out of this came out a book that has had fantastic reactions, a lot more than what we were expecting. As the writer wrote in the preface: “When nothing seems to be in favor, there is still an unknown inner strength left, a never seen before resilience, an unbelievable ability to overcome, a selfless and unconditional love that no one imagined possible… (…) With more or less difficulties, you are able to discover a new life path, with the goal of accepting what seemed unacceptable. (…) And, if in a sea of physical, emotional, social, familiar, logistic and financial problems, there are those who are able to turn their lives around and find the inner peace and sense of life that most human beings look for, that means it is possible to survive, it is possible to win, it is possible to restart!”.
The book was published on the National Stroke Survivor Day (31st March) and had a formal launch on the last Portugal AVC Meeting (13th April).
It’s one step further in the path of Portugal AVC, who has as one of the main goals to support the stroke survivors in the path of rehabilitation and integration, as complete as possible!
About Portugal AVC
Founded on September 23rd, 2016, the Portugal AVC represents the 1st national associative entity led by stroke survivors of stroke. It includes stroke survivors’ family members, as well as health professionals, caregivers and friends who embrace this cause.
The Portugal AVC is made by and with stroke survivors, who cover three out of five positions in the Executive Board, including the President.
Photo credit: Portugal AVC

Apr 19, 2019
“There is no stroke rehabilitation center in Kutaisi, Georgia, and after their hospital treatment, patients are discharged to go home. Unfortunately, patients’ carers do not have enough information on how to take care of them once their loved ones are back home. Due to swallowing problems, many of stroke survivors return to the hospital very soon after their discharge, this time not because of stroke, but because of aspiration pneumonia- a type of lung infection that is due to a relatively large amount of material from the stomach or mouth entering the lungs” says Tamar Janelidze, MD, neurologist, co-founder and board member of Georgian stroke support organization, Medical Foundation Mkurnali.
SAFE: What is one issue related to the life after stroke in your country that you think needs special attention?
TJ: In Georgia, there is an observed growth trend in cerebrovascular diseases. For last years, at the national health sector level, special attention is paid to acute strokes. In general, stroke is one of the main causes of disablement of the population of Georgia. In particular, most of patients that survived stroke are disabled, and 30-40% of them needed permanent care. Because of a deficiency in rehabilitation services in Georgia, no correction of neurological impairment can be made completely for stroke patients that reduces the quality of life. In response to the urgency of this disease, it is very important to study the methods for fighting this disease and for the management of its complications, as well as for its proper diagnosis.
In Georgia, at our hospital, at the premises of the neurology department, there have been established the stroke management units, the so-called stroke units, which allow not only for effective treatment of stroke patients, but also for assessing the complications and possible risks associated with stroke. 65% of patient had dysphagia, which evolves as a result of infringement of brain blood circulation, and appears as inhibition of swallowing reflex, or as its complete elimination.
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
TJ: There is the risk of an aspiration of foods in the airway that consequently may lead to aspiration pneumonia. Our organization contributes to the introduction of dysphagia screening in the neurology department, which include the studies were actively started for the detection of dysphagia. First, swallowing reflex is checked and lingual condition is assessed in all patients, as well as there is differentiated whether dysphagia is a neurological complication or not. Then the studies are carried out through video-photofluorography roentgenoscopy. Patient swallows the contrast substances of different consistencies, and radiologist assesses radioscopically the swallowing process. Also, in some cases, of high importance is to assess the pharynx condition, for which we apply to an endoscopy.
After the mentioned examination, an attending physician and radiologist make decision on how the dietary regime of patient should be carried out. Of all 120 examined patients, dysphagia was detected in 85, and an appropriate examination regime and treatment were chosen for them, and in some of them the need of gastrostomy was identified. Analysis of latest data has shown that the problem of proper diagnosis of dysphagia allows for reducing the complications, even such as aspiration pneumonia that in turn is the most dangerous complication in terms of mortality.
Thus, proper diagnosis is a guarantee of preventing possible disablement and anticipated mortality.
SAFE: Please tell us more about your organisation.
TJ: Our organization participates in s patient’s educational program not only for stroke patients. We also have relations with government of Kutaisi and also Kutaisi University and try together to make our patients’ lives better.

Apr 19, 2019
Author: Nora Mork
People with a chronic pain are constantly facing obstacles and difficulties that they otherwise wouldn’t. However, this doesn’t have to mean that it’s impossible to have a full and satisfying life even with the chronic pain.
You just have to learn to live with it properly and avoid making these common mistakes:
Allowing Fear To Rule Your Life
Fear is understandable in this situation but what is not is allowing it to rule your life. You are still you and there are always ways to fix this situation. There are medications available and many other things that could help you overcome your pain and have a regular life. Certainly, nothing will go back to being completely normal but maybe you should embrace your new normal instead.
Misusing the Pain Meds
Pain medication should never be used to completely block your pain. This is impossible because those pain medications become ineffective over time. They can be really helpful but it all depends on how you use them and what you expect will happen because of them.
Pain medications can only remove about 50 to 60 percent of pain. You’ll have to use other things as well to support the meds. You have to learn to live with a certain amount of pain.
You should also avoid using the pain meds to do more and get through certain things. You can’t move too fast in your recovery process and end up having more pain than before. Stick to the schedule and what your doctor told you.
Overwhelming yourself when you are feeling okay
At times you’ll feel a lot better – almost like normal – and you’ll realize that these are the times that you can do things like you used to. Soon, you’ll increase the amount of work you do during “good times”.
But this will only increase your amount of pain and result in you not being able to fix it later. Never overwhelm yourself when you are feeling good. Take frequent breaks and rest often – sit or lay down, change your position as necessary and don’t do the extremely difficult things.
Find the right kind of help
“Pain management counselors can really help you learn pain management techniques and how to move on with your life properly. Don’t think that the relief can only come from pills. You have to learn other, more effective and natural ways of managing your pain. And you can really learn a lot from these professionals,” says Hannah Thomas, a psychology blogger at Academized and Australian help.
But, you also have to learn to rely on yourself – physicians are there for you but they are there to teach you how to handle yourself and your pain, not to be available to you any time of day or night. They also can’t always understand what you are going through.
This is why you have to understand to rely on yourself but also find a support group that can help you with their experiences and so on.
Not learning about your patterns
 As you go through the process of being in a severe pain through feeling just small amounts of pain, you will learn to understand and recognize your patterns. For instance, when it happens and what happens. Ask yourself whether some fears or certain emotions make things better or worse for you. If some people have an effect on your pain – be it a good one or a bad one.
As you go through the process of being in a severe pain through feeling just small amounts of pain, you will learn to understand and recognize your patterns. For instance, when it happens and what happens. Ask yourself whether some fears or certain emotions make things better or worse for you. If some people have an effect on your pain – be it a good one or a bad one.
Then, you can learn to avoid of milden these effects. This is a great way to learn to live – in part – with the pain.
Thinking that you can’t go on
“Everyone sometimes feels like they can’t keep living in pain and they feel desperate but they are wrong. People can survive anything and still have a full and happy life with pain.
So, learn to live with it and overcome it in difficult situations,” says Milo Banks, a health writer at Big Assignments and State of writing.
Failing to refill your prescription
For one, you need to remember to always refill your prescription – meds aren’t the only pain management that you should use but they should still be a part of it. Failing to do so will only result in your recovery slowing down.
You should also remember to refill it in time – for example, never let your meds run out during the weekend or holidays, get a prescription before that. The doctors have their own lives which they shouldn’t have to stop in order to get to you because of your mistakes.
Having chronic pain is scary but it’s also possible to have a good life with this illness. Hopefully, you’ll avoid these mistakes and have a good life.
About the author: Nora Mork is a health and psychology writer and editor at UK Writings. She helps people by sharing her experience in the articles at Boom Essays and Essay Roo blogs.

Apr 17, 2019
This article was first published on ESO website | Author: Giuseppe Reale, MD – ESO YSPR Committee
Same stroke, same treatment and lower limb weakness, but forget about upper motor neurons!
Sometimes it seems that stroke treatment is all about time, tissue and recanalization, whatever it takes. However, it is important to remember that danger might be just around the corner, even after a successful recanalization.
A 66-year old man was carried to our Emergency Department 4 hours after the acute onset of right hemiplegia and aphasia. CT-Angiography (CTA) showed a M1 left middle cerebral artery (MCA) occlusion and the patient underwent to systemic thrombolysis followed by mechanical thrombectomy in general anesthesia with right femoral access. When the patient was admitted to the Stroke Unit, he presented only right lower limb weakness, being able to flex the thigh at hip, but not to extend the leg at knee. The right patellar tendon reflex was absent, while the left was elicitable. The segmental weakness pattern and the reflex asymmetry suggested a femoral neuropathy. CTA of lower extremities excluded the presence of iliacus hematoma or femoral artery aneurysm. The patient had a spontaneous recovery of the neurological deficits within one week. The electromyography performed three weeks later did not show any finding of denervation at the quadriceps muscle, suggesting a previous femoral neuropraxic block.
An 82-year old woman with the same symptoms and radiological findings of the previous patient underwent thrombolysis and thrombectomy with right femoral access in general anesthesia.
When transferred to the Stroke Unit, she presented just a mild drift of the right lower limb, but the day after she developed a complete plegia of the right lower limb associated with “mild pain and an unpleasant cold sensation”. The right lower limb was cold and distal pulses were absent. CTA of the lower extremities demonstrated a pseudoaneurysm of the common femoral artery, associated with distal arterial occlusion. The patient underwent emergency femoral endarterectomy without any complication.
You can read the full article here.




 SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?
SAFE: What would be the solution, i.e. what is your organisation’s position regarding this issue?

 We started with posting on Facebook 2 or 3 testimonies, that arrived to us, of people describing their post-stroke life. We quickly realized that these were the most read posts and that they had incredible reactions: We were contributing, with concrete examples, all very different among them, to the motivation of other stroke survivors!
We started with posting on Facebook 2 or 3 testimonies, that arrived to us, of people describing their post-stroke life. We quickly realized that these were the most read posts and that they had incredible reactions: We were contributing, with concrete examples, all very different among them, to the motivation of other stroke survivors!

 As you go through the process of being in a severe pain through feeling just small amounts of pain, you will learn to understand and recognize your patterns. For instance, when it happens and what happens. Ask yourself whether some fears or certain emotions make things better or worse for you. If some people have an effect on your pain – be it a good one or a bad one.
As you go through the process of being in a severe pain through feeling just small amounts of pain, you will learn to understand and recognize your patterns. For instance, when it happens and what happens. Ask yourself whether some fears or certain emotions make things better or worse for you. If some people have an effect on your pain – be it a good one or a bad one.



