Jul 17, 2018
Having a stroke is a terrifying experience, and it is only natural to start experiencing some symptoms of anxiety and depression when it is all over. After all, it is something that often brings a person close to death, and it can seem like no one else understands the feelings of fear and despair that often accompany survival. While you often feel thankful that you were able to make it through, there is nothing wrong with the negative feelings that come with it. Here is how your canine companion can help you get through this tough phase after a stroke.
Alleviating Anxiety and Depression
These are natural things to feel after a stroke, but a dog can help you get through them. Petting and hugging them releases oxytocin throughout the body, and this is the hormone responsible for reducing anxiety and stress, blood pressure, and heart rate, so you feel more relaxed and a lot less worried. They also bring comfort as a whole because you know they are always there when you need them.
They give you a sense of purpose and validation, as well as offering unconditional love that cannot be matched by another creature on this planet. There have even been studies to suggest that they are able to help the process of balancing the serotonin levels in your brain, boosting your mood and leaving you feeling in a better mindset.
Reducing Feelings of Loneliness
Often, post-stroke life can leave a person feeling increasingly lonely, and this can happen for a number of reasons. Sometimes, a lot of attention will have been received in the hospital, and family will have made special arrangements to come visit and be there as much as possible.
However, once everything is clear, life goes back to normal, and it can leave a person feeling isolated. A dog is always there to offer love, support, and companionship, and this can bring a great deal of comfort, as well as reduce feelings of loneliness and isolation.
Giving You Someone to Talk to
Possibly the most important thing that a dog can do for you is give you someone to talk to when you need it most. They will not judge or abandon you, regardless of how emotional you are. A shoulder to cry on, there is nothing you cannot tell them – especially as they will never tell anyone else. Linking to the fact that they can help with loneliness, it is important to have someone to speak to in these circumstances, and sometimes another human is not the easiest or best choice for you. A dog can offer just as much, and more.
To Conclude
If you found this interesting and would like to learn more about the ways in which a dog can help with mental health, feel free to check out this detailed resource. Dogs are some of the greatest companions we could ever ask for, and as little as we give them, they always return it tenfold. We understand the struggle that comes after a stroke, and your dog is there to help you through the darkest moments in every way they can.
About the Author

Will Tottle
Will Tottle is a freelance writer, his blog can be seen here . If you are interested in more information on the benefits of dog ownership including health tips, buyer’s guides and gear reviews, then check out his guides over at Dogowner.co.uk
Follow on Facebook or Twitter

Jun 24, 2018
First appeared on ScienceDaily.com
Paralysis of an arm and/or leg is one of the most common effects of a stroke. But thanks to research carried out by scientists at the Defitech Foundation Chair in Brain-Machine Interface, in association with other members of EPFL’s Center for Neuroprothetics, the Clinique Romande de Réadaptation in Sion, and the Geneva University Hospitals, stroke victims may soon be able to recover greater use of their paralyzed limbs. The scientists’ pioneering approach brings together two known types of therapies — a brain-computer interface (BCI) and functional electrical stimulation (FES) — and has been published in Nature Communications.
“The key is to stimulate the nerves of the paralyzed arm precisely when the stroke-affected part of the brain activates to move the limb, even if the patient can’t actually carry out the movement. That helps reestablish the link between the two nerve pathways where the signal comes in and goes out,” says José del R. Millán, who holds the Defitech Chair at EPFL.
Twenty-seven patients aged 36 to 76 took part in the clinical trial. All had a similar lesion that resulted in moderate to severe arm paralysis following a stroke occurring at least ten months earlier. Half of the patients were treated with the scientists’ dual-therapy approach and reported clinically significant improvements. The other half were treated only with FES and served as a control group.
For the first group, the scientists used a BCI system to link the patients’ brains to computers using electrodes. That let the scientists pinpoint exactly where the electrical activity occurred in the brain tissue when the patients tried to reach out their hands. Every time that the electrical activity was identified, the system immediately stimulated the arm muscle controlling the corresponding wrist and finger movements. The patients in the second group also had their arm muscles stimulated, but at random times. This control group enabled the scientists to determine how much of the additional motor-function improvement could be attributed to the BCI system.
Reactivated tissue
The scientists noted a significant improvement in arm mobility among patients in the first group after just ten one-hour sessions. When the full round of treatment was completed, some of the first-group patients’ scores on the Fugl-Meyer Assessment — a test used to evaluate motor recovery among patients with post-stroke hemiplegia — were over twice as high as those of the second group.
“Patients who received the BCI treatment showed more activity in the neural tissue surrounding the affected area. Due to their plasticity, they could help make up for the functioning of the damaged tissue,” says Millán.
Electroencephalographies (EEGs) of the patients clearly showed an increase in the number of connections among the motor cortex regions of their damaged brain hemisphere, which corresponded with the increased ease in carrying out the associated movements. What’s more, the enhanced motor function didn’t seem to diminish with time. Evaluated again 6-12 months later, the patients hadn’t lost any of their recovered mobility.
Story Source: Ecole Polytechnique Fédérale de Lausanne. “A dual-therapy approach to boost motor recovery after a stroke.” ScienceDaily. ScienceDaily, 20 June 2018. <www.sciencedaily.com/releases/2018/06/180620094808.htm>.
Jun 20, 2018
First appeared on oruen.com
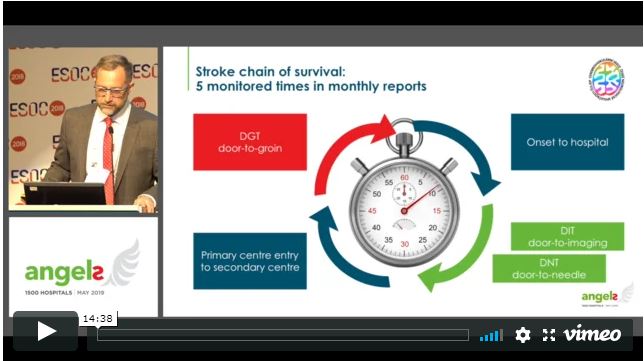
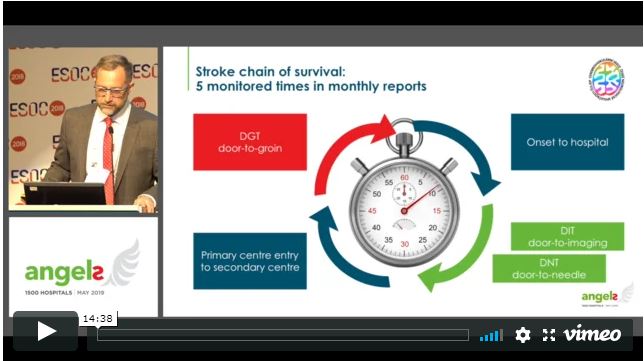
Every 30 minutes a stroke patient who could have been saved, dies or is permanently disabled, because they were treated in the wrong hospital.
Angels Initiative is building a global community of stroke centers and stroke-ready hospitals, working every day to improve the quality of treatment for every stroke patient.
The goal is to get 1500 stroke-ready hospitals around the world by May 2019.
Please click on the photo bellow to access the series of the Angels ESOC 2018 symposium videos:

For more information about Angels Initiative, please visit www.angels-initiative.com
Jun 19, 2018
First appeared on ScienceDaily.com
For every three individuals who have had a stent implanted to keep clogged arteries open and prevent a heart attack, at least one will experience restenosis — the renewed narrowing of the artery due to plaque buildup or scarring — which can lead to additional complications.
Now, a team led by UBC electrical and computer engineering professor Kenichi Takahata has developed a type of “smart stent” that monitors even subtle changes in the flow of blood through the artery, detecting the narrowing in its earliest stages and making early diagnosis and treatment possible.
“We modified a stent to function as a miniature antenna and added a special micro-sensor that we developed to continuously track blood flow. The data can then be sent wirelessly to an external reader, providing constantly updated information on the artery’s condition,” said Takahata.
The device uses medical-grade stainless steel and looks similar to most commercial stents. Researchers say it’s the first angioplasty-ready smart stent — it can be implanted using current medical procedures without modifications.
Research collaborator Dr. York Hsiang, a UBC professor of surgery and a vascular surgeon at Vancouver General Hospital, noted that monitoring for restenosis is critical in managing heart disease.
“X-rays such as CT or diagnostic angiograms, which are the standard tools for diagnosis, can be impractical or inconvenient for the patient,” said Hsiang. “Putting a smart stent in place of a standard one can enable physicians to monitor their patient’s health more easily and offer treatment, if needed, in a timely manner.”
The device prototype was successfully tested in the lab and in a swine model. Takahata, who holds patents for the technology, says his team is planning to establish industry partnerships to further refine the device, put it through clinical trials and eventually commercialize it.
Story Source: University of British Columbia. “‘Smart stent’ detects narrowing of arteries.” ScienceDaily. ScienceDaily, 19 June 2018. <www.sciencedaily.com/releases/2018/06/180619123000.htm>.

Jun 11, 2018
First appeared on ScienceDaily.com
Stroke is the most common cause of adult disability. This is due not only to the high incidence of stroke, but also because spontaneous recovery is often incomplete and no drugs are available that hasten recovery.
Mesencephalic astrocyte-derived neurotrophic factor MANF is neuroprotective when administered before experimental stroke in rats.
A massive immune response mediated by activated microglia and macrophages occurs in the rat brain tissue after stroke. MANF has also recently been shown to recruit immune cells to the eye after retinal damage and to mediate retinal repair after photoreceptor transplantation.
Dr. Mikko Airavaara and his group at the University of Helsinki, Institute of Biotechnology administered MANF to rats after the ischemic brain injury, either by injecting recombinant MANF protein or by delivering a MANF-expressing viral vector into the brain area adjacent to the lesion.
When MANF was administered directly into brain tissue 2 to 3 days after stroke, it did not affect lesion volume but promoted reversal of stroke-induced behavioural impairments. “This indicated that MANF had an effect on the recovery of brain tissue function after injury,” says Dr. Kert Mätlik, the lead author of the study.
MANF treatment transiently increased the number of phagocytic macrophages close to the ischemic lesion. These cells are the professional cleaning crew that clears dying cells and dead material from injured tissue. “This really got me wondering if some of the inflammation is beneficial. What if facilitating specific branches of the inflammatory response enhances both tissue repair and functional recovery?” asks Mikko Airavaara.
By virtue of the presence of a skilled neurosurgeon, Dr. Kuan-Yin Tseng in the lab and a collaboration with Dr. Maria Lindahl, the researchers were also able to study the outcome of experimental stroke in mice that lack MANF in their brain cells. These additional experiments revealed the neuroprotective effect of endogenously-produced MANF against ischemic injury.
Mikko Airavaara has found the results very encouraging for pursuing the ultimate goal of combating long-term disability in stroke patients: “All in all this is a proof-of-concept study that shows the beneficial effect of MANF treatment on the reversal of stroke-induced behavioural deficits. It suggests that MANF or therapeutic agents with similar activity could be developed to repair brain tissue after stroke. However, much more work is needed before clinical studies can be considered.”
Story Source: University of Helsinki. “Post-stroke delivery of neurotrophic factor MANF promotes functional recovery in rats.” ScienceDaily. ScienceDaily, 11 June 2018. <www.sciencedaily.com/releases/2018/06/180611133731.htm>.
Jun 8, 2018
First appeared on ScienceDaily.com
More than 2.5 million Americans are living with Atrial Fibrillation (AFib). AFib is an irregular heartbeat that can lead to blood clots, stroke, heart failure and other heart-related complications.
What doctors and researchers currently understand about treating AFib stems mainly from whether a patient has been diagnosed with the condition or not. University of Minnesota researchers are urging the medical community to take a closer look, specifically at AFib burden.
AFib burden refers to the amount of AFib that an individual has. The goal of the scientific statement published in the American Heart Association’s journal Circulation is to increase knowledge and awareness by healthcare professionals of effective, state-of-the-art science related to the causes, prevention, detection, management, and future research needs related to AFib burden.
“We hope to bring awareness to this concept of measuring the AFib burden and then to outline what we know about it,” said Lin Yee Chen, MD, MS, tenured associate professor, Department of Medicine at the University of Minnesota Medical School, “the hope then is to use that knowledge so more research can be done to fill in those gaps.”
AFib is associated with an elevated risk of stroke, and this statement also pushes for more research to refine risk classifications for stroke. Further understanding the relationship between AFib pattern or burden and stroke risk might result in deeper insights into stroke prevention.
“We could see an enormous benefit to our patient population once these standards are applied. And now is the time to do so,” said Chen.
Story Source: University of Minnesota Medical School. “A deeper understanding of AFib could lower risk.” ScienceDaily. ScienceDaily, 6 June 2018. <www.sciencedaily.com/releases/2018/06/180606143719.htm>.