Jan 24, 2020
First published on EFNA website – Event announcement and invitation
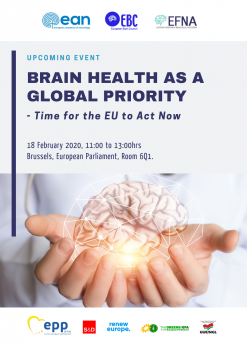
On 18 February 2020, EFNA together with EBC and EAN, will hold the event “Brain Health as a Global Priority – Time for the EU to Act Now” in the European Parliament, Brussels from 11am to 1pm in Room 6Q1, hosted by Jarosław Duda, EPP.
Follow this link to register via EFNA website.
 The event is held under the patronage of Members of the European Parliament [EP]:
The event is held under the patronage of Members of the European Parliament [EP]:
- Ewa Kopacz, Vice President of the EP, European People’s Party [EPP]
- Mairead McGuinness, Vice President of the EP, European People’s Party [EPP]
- Miriam Dalli, Vice-Chair, Group of the Progressive Alliance of Socialists and Democrats [S&D]
- Frédérique Ries, Vice-Chair, Renew Europe [RE]
- Kateřina Konečná, European United Left–Nordic Green Left [GUE/NGL]
- Tilly Metz, Group of the Greens/European Free Alliance [EFA]
The event looks to explore the following:
Is brain health a global priority?
In the Political Declaration on Non-Communicable Diseases (NCDs), which arose from the United Nations (UN) High-Level Meeting on NCDs in 2018, all Governments recognized that ‘mental disorders and other mental health conditions, as well as neurological disorders, contribute to the global burden of NCDs. It resulted in adding mental and neurological health as the ‘5th NCD’, complementing global efforts to combat cancer, CVD, diabetes and chronic respiratory diseases. This has been reinforced in the recent 2019 UN Declaration on the Universal Health Coverage, where ‘mental disorders and other mental health conditions as well as neurological disorders’ have been identified as an ‘essential component of UHC’. Additionally, the World Health Organisation (WHO) is also now building a new Brain Health team to operate from its headquarters in Geneva. The question now is how can we ensure this progress can be translated into policy action at EU and member state level?
You can access more information and agenda by following this link.
Jan 10, 2020
First published on ScienceDaily.com
Middle-aged adults with high blood pressure, Type 2 diabetes, heart disease or stroke could be at high risk for cancer and early death when sleeping less than six hours per day, according to new research published in the Journal of the American Heart Association, the open access journal of the American Heart Association.
“Our study suggests that achieving normal sleep may be protective for some people with these health conditions and risks,” said lead study author Julio Fernandez-Mendoza, Ph.D., associate professor at Pennsylvania State College of Medicine and sleep psychologist at the Sleep Research & Treatment Center of the Penn State Health Milton S. Hershey Medical Center in Hershey, Pennsylvania. “However, further research is needed to examine whether improving and increasing sleep through medical or behavioral therapies can reduce risk of early death.”
Researchers analyzed data of more than 1,600 adults (20 to 74 years old, more than half women) from the Penn State Adult Cohort who were categorized into two groups as having stage 2 high blood pressure or Type 2 diabetes and having heart disease or stroke. Participants were studied in the sleep laboratory (1991-1998) for one night and then researchers tracked their cause of death up to the end of 2016.
Researchers found:
Of the 512 people who passed away, one-third died of heart disease or stroke and one-fourth died due to cancer.
People who had high blood pressure or diabetes and slept less than 6 hours had twice the increased risk of dying from heart disease or stroke.
People who had heart disease or stroke and slept less than 6 hours had three times the increased risk of dying from cancer.
The increased risk of early death for people with high blood pressure or diabetes was negligible if they slept for more than 6 hours.
You can read the full article here.
Image: Pixabay.com
Jan 7, 2020
First published on ScienceDaily.com
A team of New Jersey stroke researchers has linked recovery of reading and language competence with cerebral blood flow in the left reading network. Their findings may contribute to new approaches to identifying and treating reading deficits after stroke. The open access article, “Cerebral perfusion of the left reading network predicts recovery of reading in subacute to chronic stroke” was epublished on August 26, 2019 in Human Brain Mapping. The authors are Olga Boukrina, PhD, and A.M. Barrett, MD, of Kessler Foundation, and William Graves, PhD, of Rutgers, the State University of New Jersey.
Despite the fundamental role of reading ability in everyday living, little research has been conducted on patterns of reading recovery after stroke, or the development of interventions to improve reading outcomes. In this study of left-brain stroke, a team of New Jersey scientists examined patterns of cerebral perfusion bilaterally, including left and right networks of brain areas important for healthy reading, the area surrounding the stroke lesion, and the corresponding contralateral area.
They enrolled 31 participants during inpatient rehabilitation, within 5 weeks of left-sided stroke. All underwent functional magnetic resonance imaging, psychometric testing, neurological examination and tests for phonological, orthographic and semantic impairments. Fifteen participants had follow-up studies at 3 months post stroke. Analysis of data from the subacute and chronic phases showed that recovery of reading and language competence correlated with increases in cerebral blood flow in the left reading network.
You can read the full article here.
Image: Pixabay.com

Jan 6, 2020
Source: European Journal of Arrhythmia & Electrophysiology. 2019;5(2):77–81
Authors: Kamal Kishor , Devendra Bisht , Sanjay Kalra
Abstract
Atrial fibrillation (AF) is one of the major causes of stroke, heart failure, sudden death and cardiovascular morbidity in the world. Management of AF, its risk factors and complications demands huge cost. The frequent hospitalisations, haemodynamic abnormalities, and thromboembolic events related to AF put a huge emotional and monetary burden on patients, so preventive strategies will be a cost-effective means of reducing this burden. Primordial prevention (i.e., intervention prior to onset of disease risk factors) should be implemented by the government, along with the food industry, to educate the public regarding the importance of a healthy diet and adherence to it. Primary prevention should focus on halting the onset of AF in targeted populations who carry risk factors for development of AF. The strategy at the secondary-prevention level includes optimal control of rate or rhythm either by anti-arrhythmic drugs or catheter ablation. Every effort should be made to reduce the incidence of ischaemic stroke by using optimal oral anticoagulation, devices or surgical closure of left atrial appendage. Tertiary level prevention should focus on the management of complications incurred as a result of AF, such as ischaemic stroke, heart failure or asymptomatic left ventricular dysfunction. Since management of AF demands a huge economic burden and the line between thrombotic complications and bleeding complications is a thin one; over-diagnosis and overtreatment of AF should be avoided. The ultimate aim of quinary prevention is to sensitise the physician to follow evidence-based medicine and to get rid of populated myth. This current review summarises a stepwise preventive strategy for AF from the primordial level to the quinary level.
You can read the full article in the latest exciting issue of European Journal of Arrhythmia & Electrophysiology – Volume 5 Issue 2 by clicking here.
Image: Pixabay.com
Dec 31, 2019
First published on ScienceDaily.com
In an article in Brain, researchers at the Medical University of South Carolina (MUSC) and elsewhere report which brain regions must be intact in stroke survivors with aphasia if they are to perform well in a speech entrainment session, successfully following along with another speaker.
Aphasia is the inability to speak, write or understand spoken or written language. One of the main causes of aphasia is stroke, the third leading cause of death in the U.S. About one in three stroke survivors develops aphasia.
Patients with non-fluent aphasia speak in short, halting, telegraphic sentences and have trouble forming their words. However, they often understand language relatively well.
“Speech entrainment is asking the person to repeat in real time what they hear and see, or in other words to copy the speech of another speaker,” said Leonardo Bonilha, M.D., Ph.D., who led the study. Bonilha is the SmartState® Endowed Chair for Brain Imaging and an associate professor in the Department of Neurology at MUSC.
Bonilha and Janina Wilmskoelter, Ph.D., a postdoctoral fellow at MUSC, collaborated closely with Julius Fridriksson, Ph.D., professor in the Arnold School of Public Health at the University of South Carolina and director of the Center for the Study of Aphasia Recovery (C-STAR). Other team members include C-STAR collaborators from Johns Hopkins University and the University of California, Irvine.
Speech therapy can be effective in helping stroke survivors communicate better, but non-fluency is one of the hardest symptoms to treat. Speech entrainment is an experimental approach for non-fluent aphasia in which stroke survivors practice speech production in real time by following along with another speaker.
However, not all patients with non-fluent aphasia can follow along with another speaker, suggesting that they might not benefit from speech entrainment therapy should it one day be approved for use in the clinic. Before this study, researchers did not know why some stroke survivors could follow along with another speaker and others could not.
The multi-institutional team of aphasia researchers studied which brain structures were associated with successful speech entrainment. They found that the left lateral temporal cortex needs to be intact for a stroke survivor to successfully follow along with another speaker.
“Our finding helps us understand better what are the neural mechanisms associated with the ability to have one’s speech entrained,” said Bonilha.
Read the full article here.
Image: Pixabay

Dec 28, 2019
First published on ScienceDaily.com
An advanced Magnetic Resonance Imaging (MRI) brain scan analysis in patients with stroke-related, small vessel disease helped predict problems with thinking, memory and even dementia, according to new research published in Stroke, a journal of the American Stroke Association, a division of the American Heart Association.
When a stroke or other disease damages tiny blood vessels in the brain, the condition is known as small vessel disease. This condition is the most common cause of thinking problems (planning, organizing information and processing speed) and can even lead to dementia. Although early treatment could help patients at risk, no effective test is available to identify them.
This study evaluated the accuracy of a new MRI analysis technique using diffusion tensor imaging (DTI), in predicting thinking problems and dementia related to small vessel disease. A single scan measured the brain in fine detail to reveal damaged areas. By comparing these images to a healthy person’s, researchers were able to classify the brain into areas of healthy versus damaged tissue.
Results showed that participants with the most brain damage were much more likely to develop thinking problems. The analysis also helped predict three-fourths of the dementia cases that occurred during the study.
“We have developed a useful tool for monitoring patients at risk of developing dementia and could target those who need early treatment,” said senior author Rebecca A. Charlton, Ph.D., department of psychology at Goldsmiths, University of London, in the United Kingdom.
The study included 99 patients with small vessel disease caused by ischemic stroke, a type of stroke that blocks the blood vessels deep within the brain. Slightly more than one-third were female, average age 68, and most were Caucasian. All participants were enrolled in the St George’s Cognition and Neuroimaging in Stroke (SCANS) study from 2007 to 2015 in London.
Participants received the MRI scans annually for three years and thinking tests annually for five years. Eighteen participants developed dementia during the study, with an average time to onset of approximately three years and four months.
You can read the full article here.
Image: Pixabay

 The event is held under the patronage of Members of the European Parliament [EP]:
The event is held under the patronage of Members of the European Parliament [EP]: