Dec 6, 2019
First published on ScienceDaily.com
The high levels of environmental noise we are subjected to in large cities can increase both the severity and consequences of an ischaemic stroke. More precisely, researchers from the Hospital del Mar Medical Research Institute (IMIM) and doctors from Hospital del Mar, together with researchers from the Barcelona Institute for Global Health (ISGlobal), CIBER in Epidemiology and Public Health (CIBERESP), and Brown University, in the United States, put the increased risk at 30% for people living in noisier areas. In contrast, living close to green areas brings down this risk by up to 25%. This is the first time that these factors have been analysed in relation to stroke severity. The study has been published in the journal Environmental Research.
The researchers looked at the influence of noise levels, air pollution (particularly suspended particles smaller than 2.5 microns; PM2.5), and exposure to green areas on nearly 3,000 ischaemic stroke patients treated at Hospital del Mar between 2005 and 2014. To do this, they used data from the Cartographic Institute of Catalonia, as well as models to analyse atmospheric pollutant levels, the noise map of Barcelona, and satellite images to define areas with vegetation. Also taken into account was the socioeconomic level of the place the patients lived.
Dr. Rosa María Vivanco, from the IMIM’s Neurovascular Research Group and first author of the study, points out that the study gives us initial insight into how noise levels and exposure to green spaces influences the severity of ischaemic stroke. “We have observed a gradient: the more green spaces, the less serious the stroke. And the more noise, the more serious it is. This suggests that factors other than those traditionally associated with stroke may play an independent role in the condition,” she explains. At the same time, Dr. Xavier Basagaña, one of the authors of the study and a researcher at ISGlobal, a centre supported by “la Caixa,” stresses that “exposure to green spaces can benefit human health through various mechanisms. For example, it can reduce stress, encourage social interaction, and increase levels of physical activity.” However, in this study no link was seen with atmospheric pollution. The researchers warn that one of the limitations of the work was the lack of variability in pollutant concentrations to which the study population is exposed. This made it difficult to draw conclusions, and they point out that more studies are needed in this field.
More noise, greater stroke severity
“Previous studies have demonstrated that living in places with high levels of air pollution or noise, or with fewer green areas, exposes the population to a higher risk of suffering an ischaemic stroke. This work broadens our knowledge in this field, showing that the place where we live affects not only the risk of suffering a stroke, but also its severity if it occurs,” explains Dr Gregory A. Wellenius, from the Epidemiology Department at Brown University and final author of the study. In this sense, the results indicate that patients living in noisier areas presented more severe strokes on arrival at hospital.
You can read the full article here.

Dec 5, 2019
First published on ScienceDaily.com
A major UConn School of Medicine study published in the American Heart Association’s flagship journal Circulation shows that more aggressively controlling daily blood pressure in older adults can improve brain health.
It’s been estimated that approximately two-thirds of people over the age of 75 may have damaged small blood vessels in the brain which are visible as bright white lesions on brain imaging. Prior research evidence has linked increased amounts of these white matter lesions in the brain with cognitive decline, limited mobility such as a slower walking speed, increased incidence of falls and even increased stroke risk.
The clinical trial, led by Drs. William B. White of the Calhoun Cardiology Center and Leslie Wolfson of the Department of Neurology, followed 199 hypertension patients 75 years of age and older for 3 years.
Throughout that time, researchers tracked the potential benefits of using an intensive anti-hypertensive medication treatment regimen to garner a 24-hour systolic blood pressure target of less than 130 mmHg compared to standard control (approximately 145 mmHg).
As part of the INFINITY (Intensive Versus Standard Ambulatory Blood Pressure Lowering to Prevent Functional Decline In the Elderly) study, researchers assessed the older adults’ mobility, cognitive function, their brain’s white matter progression with magnetic resonance imaging (MRI), and tracked the occurrence of any adverse events.
While the researchers did not identify any significant differences in cognitive outcomes or walking speed between the two study groups, they did observe a significant reduction in the accumulation of brain white matter disease in those receiving the intensive treatment for blood pressure control.
“The results of INFINITY demonstrate that a lower ambulatory blood pressure goal for older adults is likely to conserve future brain function and health,” said Wolfson, professor of neurology and former chair of the Department of Neurology at UConn Health.
In fact, after three years, the accrual of white matter lesions in the brain were reduced by up to 40% in the those patients receiving the intensive blood pressure therapy compared to those who were on standard therapy.
You can read the full article here.
Dec 3, 2019
First published on ScienceDaily.com
Nagoya City University (NCU) researchers have revealed an interaction between cortico-brainstem pathways during training-induced recovery in stroke model rats, providing valuable insights for improving rehabilitation methods.
Upper limb hemiparesis often occurs after ischemic or hemorrhagic stroke. Unilateral upper extremity impairment can substantially disturb patients’ ability to complete activities of daily living. Therefore, continuous improvement of rehabilitation methods is needed to achieve more positive long-term outcomes among survivors.
Researchers at NCU have identified the dynamic recruitment of the “cortex-to-brainstem” pathways via post-stroke intensive rehabilitation and its contribution to the recovery of impaired forelimb function in intracerebral hemorrhage (ICH) model rats. This crucial finding could provide new insights enabling the improvement of rehabilitative methods for humans.
Stroke often affects the primary network from the cortex to the spinal cord, causing severe ongoing motor deficits. Rehabilitation promotes the recovery of impaired motor function, which is believed to be due to reorganization of the residual neural circuits. However, how the circuits are recruited in rehabilitation-induced recovery remains unclear.
To investigate the mechanisms underlying these phenomena, the NCU team used an ICH rat model in which almost 90% of the cortico-spinal tract is destroyed, causing changes in other motor-related circuits. “We previously found abundant newly formed connections from the motor cortex to the red nucleus in rehabilitated rats,” first author Akimasa Ishida explains. “Interestingly, we also uncovered an increase in the “cortex-to-reticular formation” pathway in trained rats when the “cortico-to-red nucleus” pathway failed to function, using a double-viral infection technique during rehabilitation.”
You can read the full article here.
Nov 15, 2019
PRESS RELEASE ¦ FRIDAY, NOVEMBER 15, 2019 9:00 AM EST
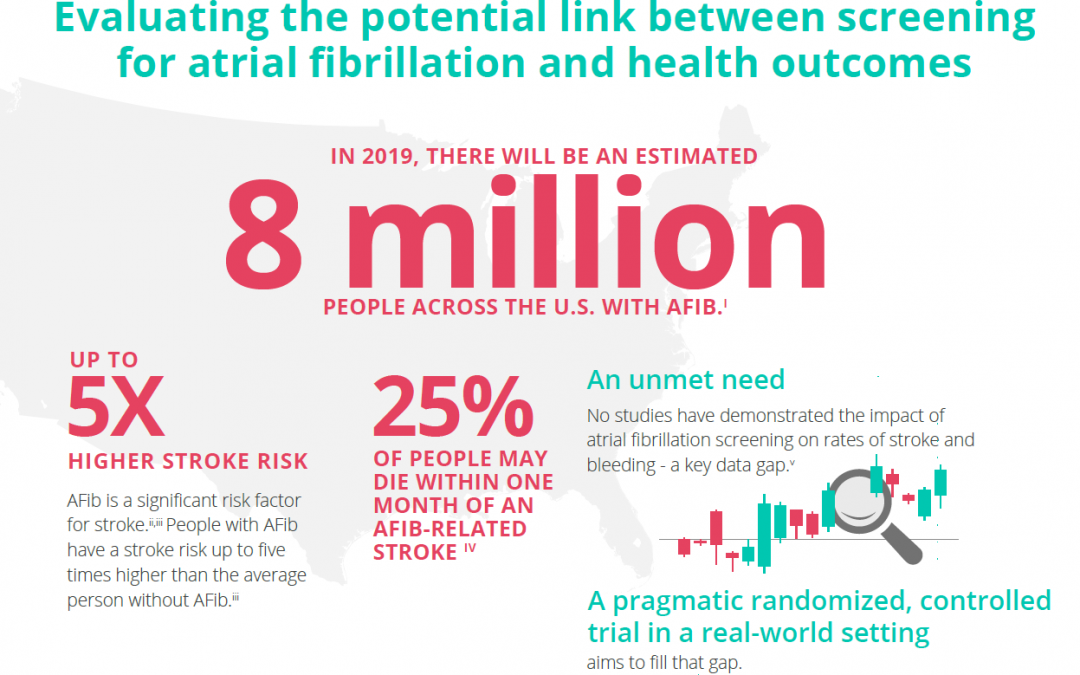
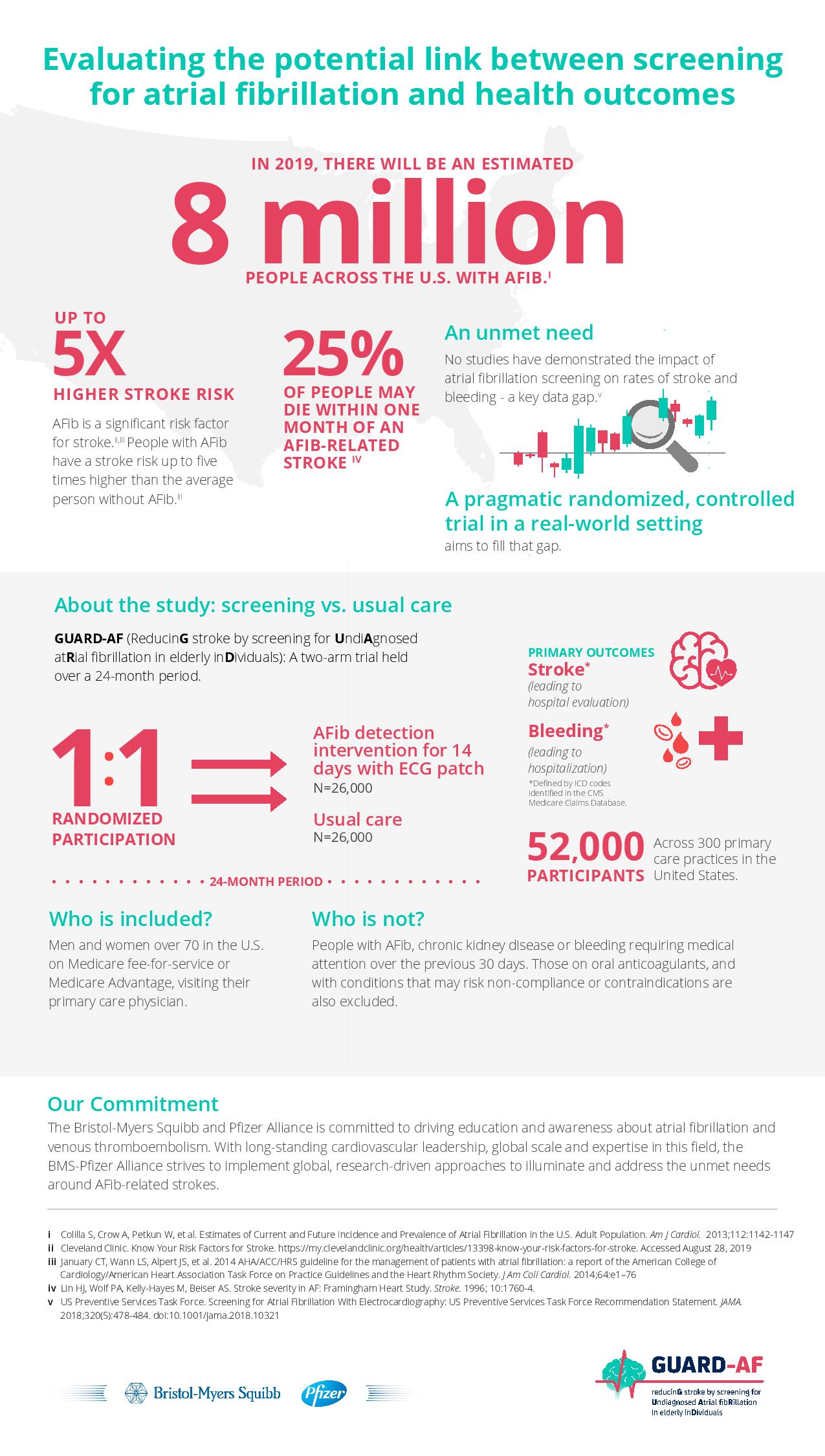
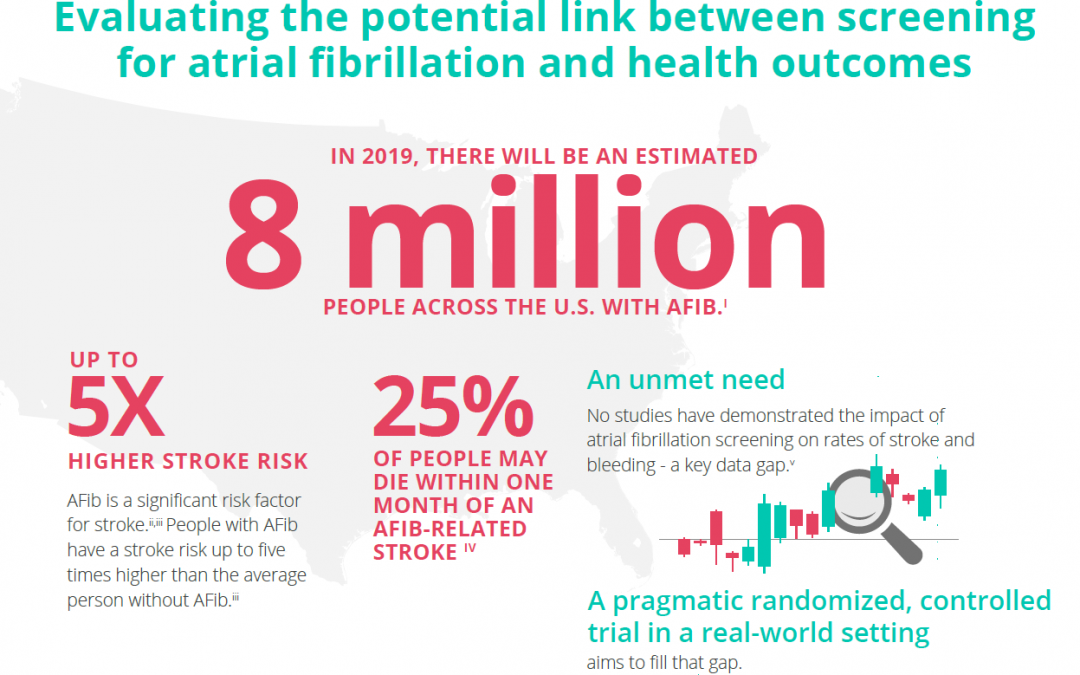
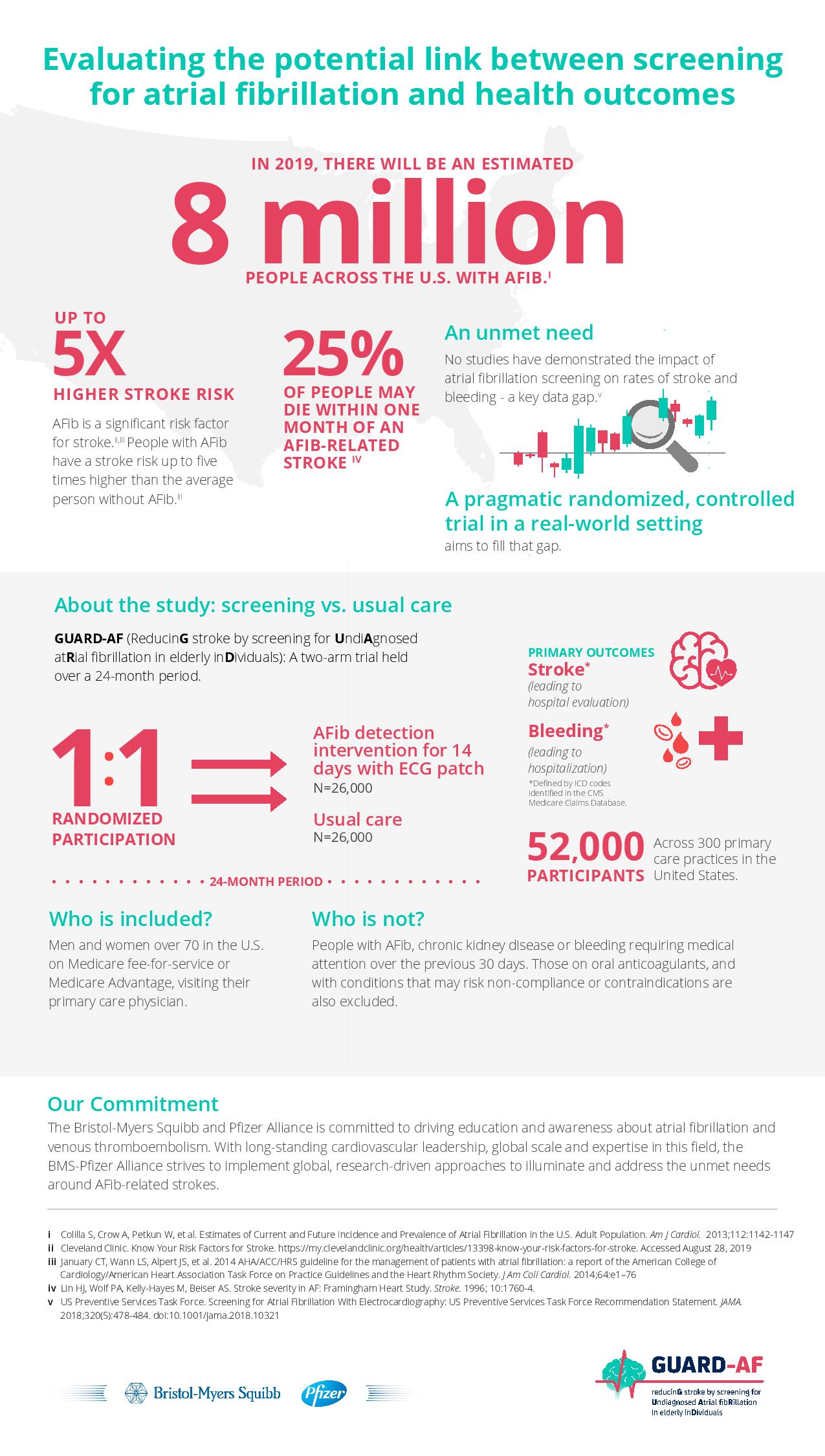
The Bristol-Myers Squibb-Pfizer Alliance today announced the initiation of a new randomized, controlled study, GUARD-AF (ReducinG stroke by screening for UndiAgnosed atRial fibrillation in elderly inDividuals). The study seeks to determine if earlier detection of atrial fibrillation (AFib) through screening in previously undiagnosed men and women at least 70 years of age in the U.S. ultimately impacts the rate of stroke, compared to usual standard medical care. This study will also assess potential bleeding leading to hospitalization, and therefore provide an evaluation of net clinical benefit or harm. AFib is the most common type of significant irregular heart rhythm, and it is estimated that 8 million people in the U.S. will be affected by AFib in 2019.i,ii AFib is a significant risk factor for stroke; stroke risk is up to five times higher in people with AFib than in those without it.iii,iv AFib can often go undetected, as it can be asymptomatic,i and some studies suggest that more than 25 percent of people who have an AFib-related stroke find out they have AFib after a stroke.v
“There is a real need for a study like GUARD-AF to assess the impact of screening for AFib on the crucially important outcome of stroke,” said Daniel Singer, M.D., Professor of Medicine at Harvard Medical School and Professor in the Department of Epidemiology at Harvard T.H. Chan School of Public Health, and an academic general internist at Massachusetts General Hospital. “This study has the potential to directly affect clinical practice and could lead to more AFib patients being identified and appropriately managed to avoid stroke.”
You can read the full press release here.
Disclaimer: This article was written by a third party. It does not necessarily express the views of the Stroke Alliance for Europe. The party who issues this press release is entirely responsible for the accuracy of its information.
Oct 25, 2019
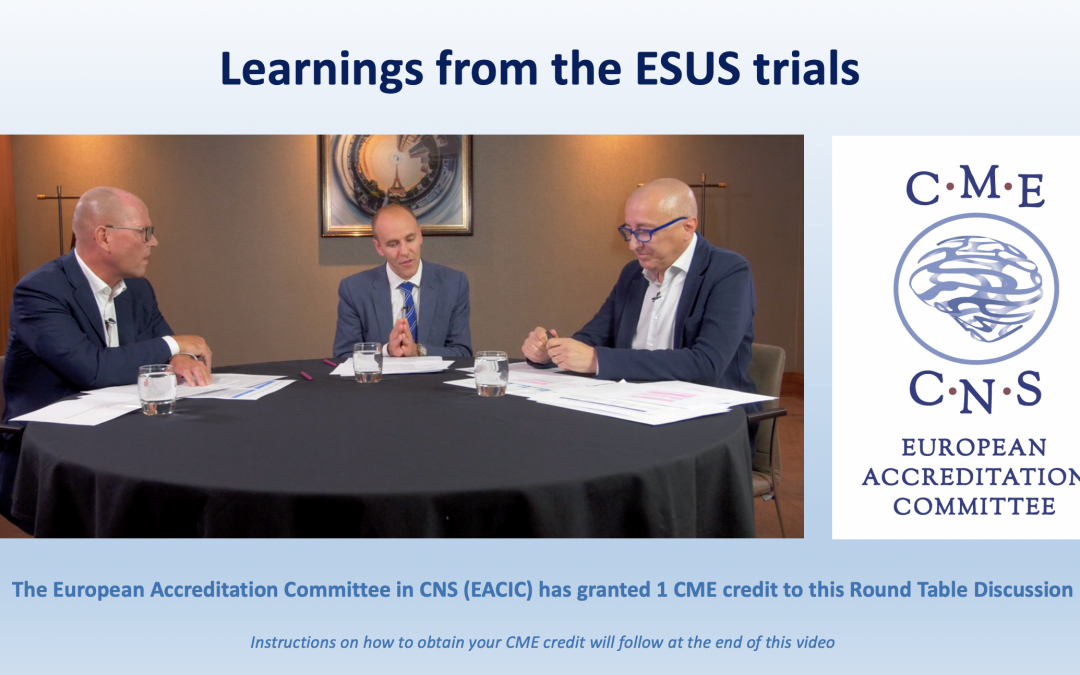
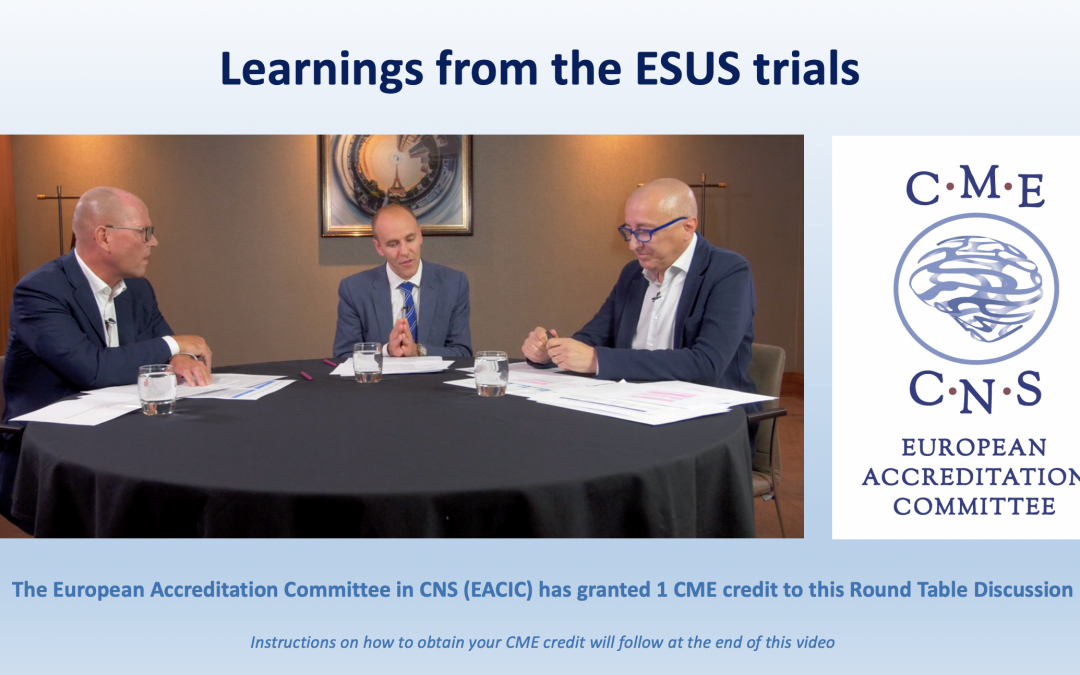
Oruen, CNS medical publication and audio-visual platform, would like to recommend to your attention the latest round table discussion about learnings from the ESUS trials – Jesse Dawson, Martin Grond & Maurizio Paciaroni.
Faculty:
Jesse Dawson MD, Professor, Institute of Cardiovascular & Medical Sciences University of Glasgow, Scotland
Martin Grond MD, Professor, Department of Neurology Kreisklinikum Siegen, Teaching Hospital of the University of Marburg, Germany
Maurizio Paciaroni MD, Neurologist, Stroke Unit and Division of Cardiovascular Medicine, Santa Maria della Misericordia Hospital, University of Perugia, Italy
This video discusses the role of NOACs for secondary prevention of stroke in the setting of embolic stroke of unknown source
Following completion of this activity, learners will be able to:
- Outline key features and results of the ESUS trials, with focus on NAVIGATE ESUS and RE-SPECT ESUS
- Recognize differences in study outcomes
- Summarise implications of ESUS as a concept for use in clinical practice

Oct 17, 2019
Leaders in atrial fibrillation and wearable technology to develop educational content around atrial fibrillation to help identify and support those at increased risk of stroke
Press Release | THURSDAY, OCTOBER 17, 2019
The Bristol-Myers Squibb-Pfizer Alliance and Fitbit today announced at the TIME 100 Health Summit in New York that they are working together to help drive timely diagnosis of atrial fibrillation (AFib) with the aim of improving earlier detection in individuals at increased risk of stroke. The BMS-Pfizer Alliance and Fitbit plan to collaborate on the development of educational content and guidance to support people at increased risk for AFib. Upon submission and U.S. Food and Drug Administration (FDA) clearance of the AFib detection software on Fitbit devices, the parties will aim to provide users with appropriate information to help encourage and inform discussions with their physicians.
“We’re in a new era of healthcare, where we’re not only focused on developing treatments but also looking at the potential of technology and data to help patients learn more about their health,” said Angela Hwang, Group President, Pfizer Biopharmaceuticals Group. “We are excited about wearables and how our work with BMS and Fitbit may potentially help patients and physicians detect and understand heart rhythm irregularities.”
AFib is the most common type of irregular heartbeat and is a significant risk factor for stroke.1,2 Approximately eight million people in the United States are projected to be affected by AFib in 2019.3 As the U.S. population ages, this number is expected to rise, as adults aged 65 and older are at an increased risk of developing the condition.3 Because AFib can be asymptomatic, it can often go undetected, and some studies suggest that more than 25 percent of people who have the condition find out after they have a stroke.(1,4)
“At Fitbit, we’re focused on making health more accessible and, through our efforts with the BMS-Pfizer Alliance, we have the potential to support earlier detection of atrial fibrillation, a potentially asymptomatic condition that affects millions of Americans,” said James Park, Co-founder and CEO of Fitbit. “With our continuous, 24/7 on-wrist health tracking capabilities, and our experience delivering personalized, engaging software and services, we believe we can develop content to help bridge the gaps that exist in atrial fibrillation detection, encouraging people to visit their doctor for a prompt diagnosis and potentially reduce their risk of stroke.”
Wearable technology has continued to become more integrated in the healthcare landscape(5) as people have recognized the value that 24/7 health tracking can have for people of any age or health status, including those at increased risk for specific conditions. Yet, those who use wearables to track their heart rhythm may lack the education or guidance on what to do with the data gathered from their device.6
“Too many people discover that they are suffering from atrial fibrillation only after experiencing a stroke. In fact, some studies suggest that this is true for more than 25 percent of people who have the condition,” said Joseph Eid, M.D., Head of Medical Affairs, Bristol-Myers Squibb. “These efforts with Fitbit exemplify not only our unwavering commitment to addressing the evolving needs of patients with atrial fibrillation, but also our dedication to advancing care by embracing technology as a part of routine clinical practice.”
Please continue reading here.
Image source: Fitbit.com